PANS/PANDAS:
RESOURCES FOR MEDICAL PROFESSIONALS
Recognizing the symptoms, knowing how to evaluate for possible PANS/PANDAS, and beginning treatment will help lay the foundation for a full recovery.
COULD STREP BE CAUSING THE PSYCHIATRIC SYMPTOMS?
The strep bacteria which produce post-infectious sequelae are often not symptomatic for pharyngitis; they produce minimal or no symptoms of sore throat, fever, abdominal pain, etc. Infections can go undetected and untreated for prolonged periods of time. Documenting a strep trigger may be difficult.
SIGNS AND SYMPTOMS OF PANS/PANDAS
Children with PANS/PANDAS have an abrupt and dramatic onset of OCD or Restrictive Eating Disorder plus additional symptoms from at least 2 of the following categories:
- Anxiety and/or separation anxiety
- Emotional lability and/or depression
- Irritability, aggression, and/or severe oppositional behaviors
- Behavioral regression
- Deterioration in school performance
- Sensory or motor abnormalities (including tics)
- Somatic signs and symptoms, including sleep disturbances or urinary frequency
QUICK FACTS
PANS (Pediatric Acute-onset Neuropsychiatric Syndrome)
- Clinically defined disorder characterized by the sudden onset of OCD or eating restrictions.
- Patients have comorbid symptoms from defined categories.
- PANS criteria does not specify a trigger. The syndrome is thought to be an immune reaction to one of a number of physiological stressors including Group A Streptococcal infection, Mycoplasma pneumonia infection, influenza, upper respiratory infections, sinusitis, and psychosocial stresses.
- PANS has no age limitation.
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections)
- PANDAS is a subset of PANS.
- There are five distinct criteria for diagnosing PANDAS, including abrupt OCD or dramatic, disabling tics; a relapsing-remitting, episodic symptom course; young age at onset (average of 6–7 years); presence of neurologic abnormalities; and temporal association between symptom onset and Group A strep infection.
- The 5 criteria usually are accompanied by similar comorbid symptoms as found in PANS.
MILD CASE:
Children with mild symptoms have obvious impairments as a result of their PANS/PANDAS symptomatology, but these are limited to certain situations or settings. The symptoms may occupy a few hours a day and may cause minor disruptions at home and in school, but these are manageable with reasonable accommodations. Overall symptom severity is in the “troubled but tolerable” range.
MODERATE CASE:
Children with moderate symptoms of PANS/PANDAS have symptoms that are distressing and interfere with daily activities. They occupy 50%–70% of waking hours. The rituals or separation anxiety may prevent the child from attending school, but would be able to go to visit grandparents (if parent is along) or have friends come over for brief periods.
SEVERE CASE:
Extremely severe cases are defined as those in which the symptoms are incapacitating, life threatening, or occupy 71%–100% of waking hours. For example, children with significant weight loss due to restrictive eating; children with extreme impulsivity, such as the child who attempts to jump off a roof because they think they can fly; or children with suicidal ideation or self-injurious behavior.
WHAT ARE THE BEST RESOURCES TO HELP ME WITH MY PATIENT?
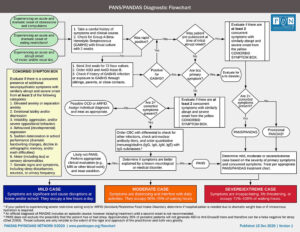
PANS/PANDAS Flowcharts
Treatment for PANS/PANDAS varies from the treatment for traditional OCD and ARFID. The flowcharts for diagnosing and treating PANS and PANDAS walk you through evaluating patients for possible PANS/PANDAS then guides you through treatment considerations based on symptom severity.
PANS Research Consortium Consensus Statement and Treatment Recommendations
“In cohorts of well-characterized PANS patients, evidence of postinfectious autoimmunity and/or neuroinflammation is found in more than 80% of cases (Swedo, et al.).” The JCAP papers include details on PANS/PANDAS treatment options including antibiotics to remove the source of inflammation (strep or other infection), anti-inflammatories, IVIG, behavioral therapies, and more.

Seeing Your First Child with PANDAS/PANS
“Seeing Your First Child with PANDAS/PANS”, by Margo Thienemann, MD, co-director of Stanford’s Immune Behavioral Health Clinic and the PPN Diagnostics and Therapeutics Committee, provides an overview and current theories, PANDAS/PANS symptoms and diagnostic criteria, workup recommendations, and expectations.
PANS/PANDAS Clinics
Pediatricians can diagnose PANS/PANDAS and implement the majority of treatments. There are a limited number of multidisciplinary care clinics available for more complex cases. Please note some clinics have strict criteria for seeing new patients due to high demand.