PANS DIAGNOSTIC GUIDELINES
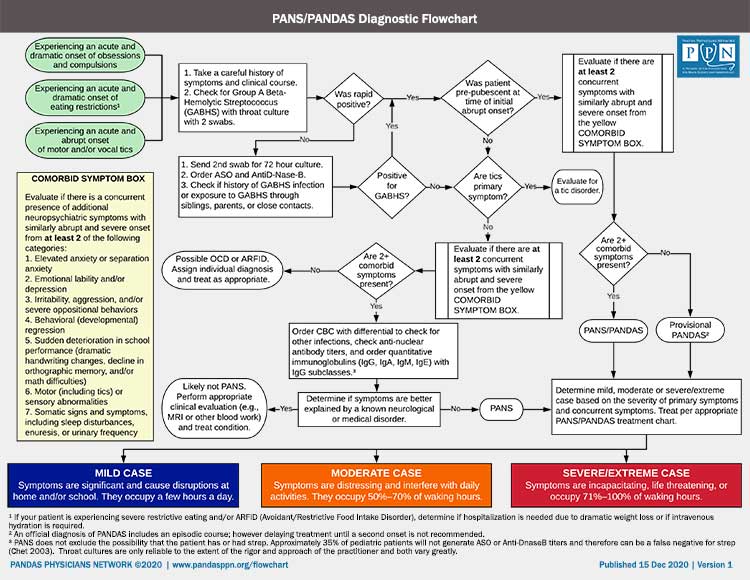
Much like the Jones Criteria for rheumatic fever, the PANS (“Pediatric Acute-onset Neuropsychiatric Syndrome”) criteria are based upon clinical presentation.
To diagnose PANS, a patient must fulfill the following criteria:
- An abrupt, acute, dramatic onset of obsessive-compulsive disorder or severely restricted food intake
- Concurrent presence of additional neuropsychiatric symptoms with similarly severe and acute onset from at least 2 of the following categories:
· Anxiety
· Emotional Lability and/or Depression
· Irritability, Aggression, and/or Severe Oppositional Behaviors
· Behavioral (Developmental) Regression
· Sudden Deterioration in School Performance
· Motor or Sensory Abnormalities
· Somatic Signs and Symptoms, including Sleep Disturbances, Enuresis, or Urinary Frequency - Symptoms are not better explained by a known neurologic or medical disorder
- Age requirement – None
There are three severity levels for PANS: Mild, Moderate and Severe. For details on each, please see additional information below.
PANS Criteria Explained
#1: An abrupt, acute, dramatic onset of obsessive-compulsive disorder or severely restricted food intake
Clinical course is characterized by the abrupt, dramatic onset of OCD and/or eating restriction along with concurrent symptoms from the list below. The onset of symptoms can often be assigned to a particular day or week. A typical patient develops symptoms within a week. It is not uncommon for patients to have an abrupt and acute onset over a 24-48 hour period. Parents can often identify the day when they “lost” their child. Symptoms may reach maximum intensity over a longer time frame.
Under the PANS criteria, a child may never have had OCD before or a child previously had low level OCD and suddenly is debilitated by it. After onset, the OCD and comorbid symptoms may continue to appear over the next few days or weeks and may grow in intensity. In many cases, each new morning seems to bring another obsession, compulsion, or comorbid symptom. Comorbid symptoms and personality changes also occur. The rapid change in the child’s portfolio of symptoms makes it even harder for the patient and his or her parents to cope. PANDAS and PANS children frequently struggle with multiple OCD symptoms at the same time, as well as multiple simultaneous comorbid symptoms.
#2: Concurrent presence of additional neuropsychiatric symptoms with similarly severe and acute onset from at least 2 of the following categories:
At least two comorbid symptoms must accompany the sudden onset of OCD or eating restrictions. (Others frequently occur shortly thereafter, but those are not a requirement of PANS.) The presenting symptoms often change over the first weeks of illness. For example, a child might start with OCD, separation anxiety, and urinary frequency, and then develop impulsivity, aggression, and cognitive changes. Click the category for a detailed description of each comorbid symptom of PANS:
- Anxiety
- Emotional Lability and/or Depression
- Irritability, Aggression, and/or Severe Oppositional Behaviors
- Behavioral (Developmental) Regression
- Sudden Deterioration in School Performance
- Motor or Sensory Abnormalities
- Somatic Signs and Symptoms, including Sleep Disturbances, Enuresis, or Urinary Frequency
#3: Symptoms are not better explained by a known neurologic or medical disorder
The third major criterion of PANS required that symptoms are not better explained by a known neurological or medical disorder such as Sydenham chorea, systemic lupus erythematosus, Tourette disorder, or others. Thus, to make the diagnosis of PANS, clinicians must perform a diagnostic evaluation that is comprehensive enough to rule out other potential disorders, including toxic effects of drugs or medications. A complete medical history and thorough physical and neurologic examination is encouraged.
#4: Age requirement- None
PANS has no age limitation, but symptoms typically begin during the grade-school years. Patients can also have their initial symptom onset during adolescence. PANDAS requires symptom onset prior to puberty. The age cap was based upon studies that indicated that 98% of 12-year-olds have immunity against strep infections and therefore could not develop post-streptococcal sequelae, such as PANDAS. However, the intent of the criteria was to define a homogeneous group of patients for research and not to preclude post-pubescent patients from receiving a PANDAS diagnosis, if all other criteria were met. In fact, numerous post-pubertal cases have been identified, including several at the NIMH.
PANS/PANDAS SYMPTOM DESCRIPTIONS
OCD
There are many different types of obsessions and compulsions, and a complete listing is not possible here. Many medical professionals assume OCD is repetitive hand washing. However, OCD consists of many types of obsessions and compulsions. For a full description of OCD, please see the International OCD Foundation website and the Y-BOCS Symptom Checklist, which includes a comprehensive list of 67 types of obsessions and compulsions. A short, but not full, list of OCD symptoms includes:
- Contamination obsessions (germs, bodily secretions or waste, poisons, animals, environmental contaminants like tobacco, cleansers or any substance). Often, the obsession leads to compulsive washing or cleaning rituals; but, in some cases, the symptoms cause the child to avoid the feared contaminant. In severe cases, even a loving parent may be a contaminant because of “exposure” to the dirty object, and the child will develop complex rituals to avoid contact with the exposed parent.
- Sexual or religious obsessions (fear that God hates them or that they have done something morally offensive)
- Aggressive obsessions of harm to oneself or others
- Repeating compulsions (examples: going in and out of a doorway; switching on/off appliances or light switches; re-reading pages over and over)
- Symmetry and exactness obsessions (examples: books and papers must be properly aligned; every action has to be done exactly the same on the right and left side; the child has to walk exactly in the center of a hallway)
- Ordering / arranging compulsions (example: suddenly placing bathroom items in a particular order and extreme anxiety if they are moved)
- Counting compulsions (examples: having to count ceiling tiles, books, or words spoken)
- Checking compulsions and requests for reassurance (examples: repeatedly asking a parent “is this okay?” or “did I do that right?”)
- Need to touch, tap, or rub (examples: rubbing the back of one’s hand across the table in a certain way, urge to touch rough surfaces)
- Intrusive images, words, music or nonsense sounds (examples: unwanted images, words, or music appear in the mind that do not stop)
- Need to tell, ask, or confess (examples: child needs to tell parent every perceived mistake or sin that day in school; excessive guilt)
- Colors, numbers, or words with special significance (examples: the color black is equated with death and anything black triggers obsessional fears; the number 3 is “lucky” and things have to be repeated three times or 3X3X3 times)
- Ritualized eating behaviors (examples: eating according to a strict ritual; not being able to eat until an exact time)
- Hoarding behaviors (Obsessional concerns about losing something important generalize to the point where nothing can be thrown away, or useless items take on special significance and cannot be discarded.)
Restrictive eating
Approximately 1 in 5 children with PANS will have restricted intake of specific foods or all food groups, often with observable weight loss and occasionally with dehydration, if fluid intake is also affected. The underlying symptom may be contamination fears associated with the food itself or what the food may have been exposed to. In some cases, obsessional fears of choking or vomiting may drive the eating restrictions. In other cases, the child refuses to eat because he fears harm will come to himself or others, such as his parents, if he eats; in these cases, the child may be afraid to speak of the association because of additional obsessional fears. Lastly, the patient may refuse to eat because of a new obsession with body image or weight. The acuity of symptom onset and age at onset can distinguish PANS-related eating restrictions from more typical anorexia nervosa.
Anxiety (heightened anxiety, separation anxiety, irrational fears)
The child may develop generalized anxiety, where he or she begins worrying about everything from the color of the sky (“How do I know that it’s really blue?”) to his health and well-being (“I don’t feel very good. Am I going to die today?”) If a child is a “worrier” by nature, there must be an abrupt and noticeable increase above baseline anxiety levels. His or her anxiety becomes consistent and increasingly disabling. Separation anxiety is also common in PANS. A previously independent child who had no problems going to his room alone, going to bed alone, or wandering away from his parents in public places, will suddenly refuse to enter his room alone, needs to sleep in his parents’ bed at night, and clings to his parent’s side in public. Even at home, the child may seek physical closeness from family members or require constant reassurance about his safety. The child may also begin questioning his own judgment and behavior, constantly asking his parent if it is okay to do routine activities. In some cases, the separation anxiety extends to inanimate objects. A child who never paid attention to the furniture may burst into tears when a table or couch is removed for sale.
The patient may also develop new phobias or irrational fears. The fears may interfere with the child’s ability to function at school, home, or with his friends. For example, he might develop a fear that he is going to get cancer and will refuse to let his mother use cleaning chemicals. Or, the child may develop fears of electrocution and refuse to walk outside because of nearby electrical wires. In other cases, there appears to be no rational basis for the phobias, such as a child who becomes deathly afraid of sitting next to a particular classmate. Children may have such overwhelming fear that they have increasingly narrow “safe zones”; in severe cases, refusing to leave their parents’ room or even their bed.
The child may develop panic attacks, with feelings of terror or dread, and physical symptoms, such as dilated pupils, racing heart, and dry mouth. Often, the “terror-stricken” look becomes part of their regular countenance, and the child seems to be continuously miserable.
Emotional Lability or Depression
An even-keeled, happy-go-lucky child may suddenly undergo a dramatic personality change and become excessively moody and emotionally labile. The child may burst into tears over problems that prior to onset would not elicit such a response. Emotionally labile children experience sudden and unexpected changes in mood, shifting from laughter to tears or anger without an obvious precipitant. The child might complain that he has an inner sense of restlessness and agitation, which is similarly inexplicable.
Some patients may experience the abrupt onset of clinical depression. A child might say “I’m not a good person,” but may also become so severe that the depression is accompanied by suicidal ideation. Self-injurious behaviors and suicidal ideation are also common and of particular concern among children with concomitant impulsivity and behavioral regression, as they may injure themselves or others. The constant battle with their own thoughts and comorbid symptoms may lead to depression until they ask “why is life worth living?”
Aggression, Irritability and Severe Oppositional Behaviors
These symptoms often top the list of parental concerns because they are so disruptive. The irritability and oppositional behaviors are present throughout the day, and the aggression occurs without provocation or precipitant. Most notable is the striking contrast between these new behaviors and the child’s usual state of being “sweet-tempered and well-behaved” or “easygoing and well-liked”. For example, a boy who has been close to his mother may suddenly begin attacking her physically, trying to hurt her. Some children recognize their irrational behavior and experience remorse after the attacks; others have no memory of the episode or their behavior. Outbursts occurring in response to interruption of an obsessional thought or compulsive ritual should not be counted as a manifestation of this category, as they are an expected occurrence among pediatric patients with severe OCD.
Behavioral (Developmental) Regression
The symptoms of developmental regression include an abrupt increase in temper tantrums, loss of age-appropriate language (sometimes to the point of the child using “baby talk”), and other behaviors inappropriate to the child’s chronological age and previous stage of development. The developmental regression may be most apparent in the child’s school assignments or artwork. Sometimes, symptoms of separation anxiety belong in this category, rather than with the anxiety disorders. The child may regress to the “clingy” stage, where he needs to be physically close to one of his parents at all times. If the separation anxiety is a manifestation of behavioral regression, it should not also be counted as an anxiety disorder.
Sudden Deterioration in School Performance
A number of factors may contribute to the child’s academic difficulties, including, among others, a shortened attention span, difficulties with concentration or memorization, and other disturbances of cognition and executive functioning. For example, a child previously may have been able to concentrate for hours on an art project, but now can focus for only a few minutes at a time. Math skills often decrease from previous levels, and children have been reported to develop new deficits of visuospatial skills.
The child may develop a number of ADHD-like symptoms, including impulsivity, inattention, and motoric hyperactivity. A child who has a high level of concentration in school or at-home activities suddenly can no longer sit still or concentrate. A child who may normally sit for a long period of time coloring his/her book can no longer stay seated longer than a few minutes. Conversely, a quick activity like tying one’s shoes suddenly takes a long time due to focus issues. The anxiety coupled with the hyperactivity may result in a changed child who is constantly alert, fidgety, and on the move. As with the other categories, the academic difficulties must represent a distinct change from previous levels of functioning. Thus, manifestations of pre-existing attention deficit hyperactivity disorder (ADHD) or learning disabilities are not counted here, nor are long-standing deficits of visuospatial or fine motor skills.
Patients in many studies score poorly on orthographic memory tests like the Rey-Osterrieth Complex Figure Test.
Motor and Sensory Abnormalities (touch, visual images, sound)
Motor abnormalities include a variety of signs and symptoms, such as an abrupt deterioration of the child’s handwriting (dysgraphia), clumsiness, tics, choreiform movements, motoric hyperactivity, and akathisia. Dysgraphia is a particularly useful diagnostic feature, as handwriting samples obtained during the child’s acute illness can be compared against those produced during an asymptomatic period. This feature of the disorder can be used to identify precipitating infections by comparing longitudinally-collected handwriting samples with infections documented in the child’s medical record. Asking the child to copy a complex picture such as a Rey-Osterrieth figure may also demonstrate abnormalities. Choreiform movements must be distinguished from choreoathetoid movements of Sydenham chorea. While chorea is characterized by jerky or writhing, arrhythmic, involuntary movements of the extremities, trunk, and facial muscles, choreiform movements are described as “fine, piano-playing movements of the fingers” that present only when the child maintains stressed postures such as arms stretched straight out, hands extended.
All tics start suddenly. One day they are not there and the next they are. But certain tics are distinguishable by their intensity and interference with daily life. Complex tics or dramatic, debilitating tics are characteristic of PANS as well as PANDAS. Tics that existed prior to onset and continued at the same rate and intensity would not qualify as meeting this comorbid criteria.
The sensory abnormalities may include a sudden increase in sensitivity to light, noises, smells, tastes, or textures. For example, the child may refuse to eat certain “stinky” foods, like cheese, or to wear scratchy, tight, or otherwise uncomfortable clothing, such as the waistband of underwear or socks. In other cases, the child may develop sensory-seeking behaviors, such as needing to touch or feel particular objects or textures.
Visual hallucinations may also occur and might include frightening images and altered perceptions, such as objects that appear to be floating or to change size, appearing larger or smaller than their actual size. The visual hallucinations are usually brief, but may be more persistent, lasting for several hours or longer. Children have described these “nightmares while awake” as extremely disturbing and frightening, such as seeing their parents killed or injured by an intruder.
Somatic Signs and Symptoms Including Sleep Disturbances, Enuresis, or Urinary Frequency
Sleep problems and disturbances of urination and micturition are among the most common physical manifestations of PANS. The sleep disturbances may include not only the new onset of terrifying nightmares and night terrors, but also difficulties falling asleep, staying asleep, or waking up too early (early, middle, or terminal insomnia). The child therefore experiences little of the fifth and final stage of the sleep cycle – REM sleep. Urinary symptoms are often the presenting complaint for children with PANDAS. A pediatric clinic-based case series reported that 7 of 12 PANDAS patients initially presented with urinary symptoms, including the new onset of nighttime bedwetting (secondary enuresis), daytime urinary frequency, and an urgency to void, without evidence of a urinary tract infection. Subsequent experience has confirmed that urinary symptoms occur frequently during recurrences, as well as at the onset of symptoms. The symptoms are occasionally related to obsessional concerns with toileting or contamination fears, but for most children, no cognitive or emotional explanation can be found.
MILD CASE
Symptoms are significant and cause disruptions at school and/or home. They occupy a few hours a day.
MODERATE CASE
Symptoms are distressing and interfere with daily activities. They occupy 50%-70% of waking hours.
SEVERE CASE
Symptoms are incapacitating, life threatening, or occupy 71%-100% of waking hours.