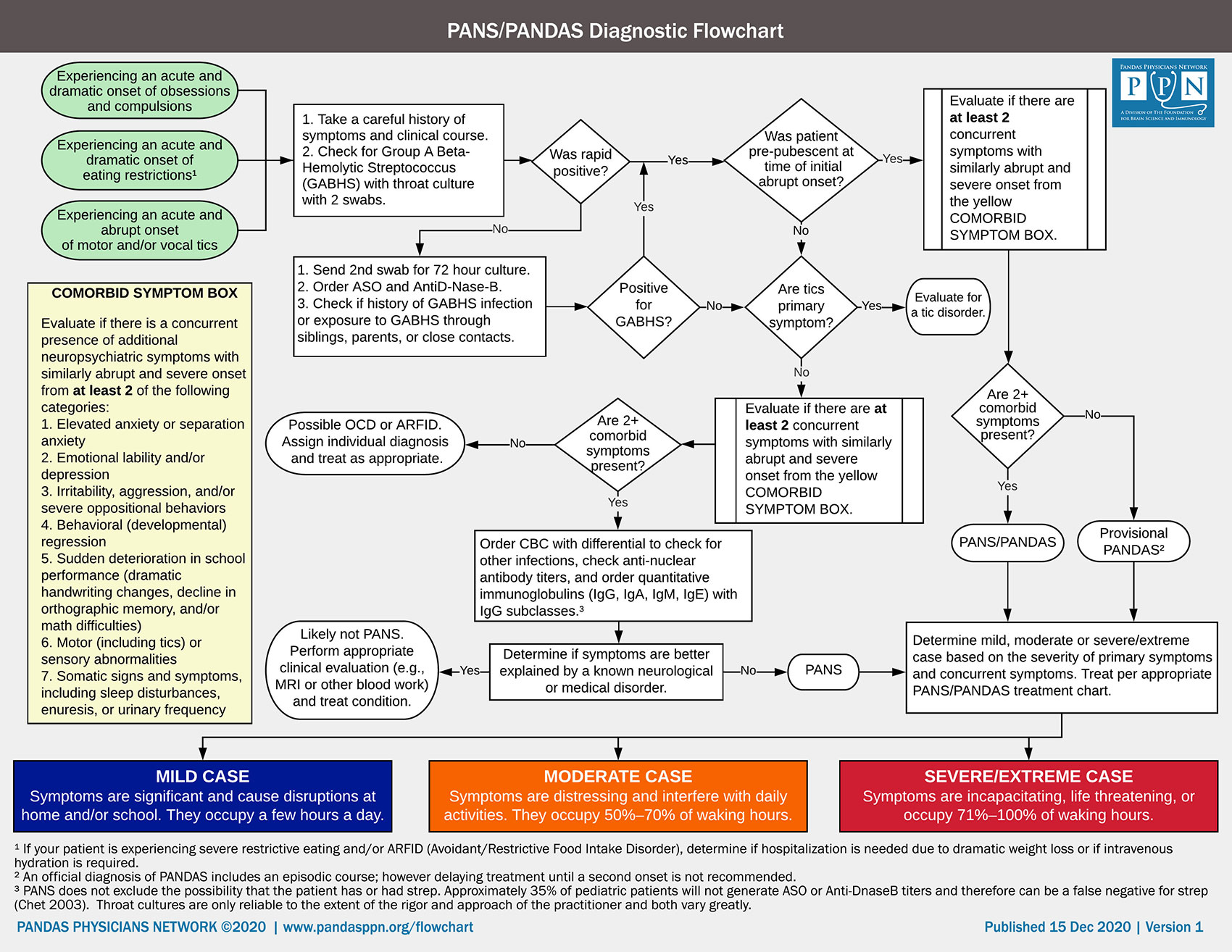
Diagnostic Flowchart and Treatment Guidelines
The PANDAS Physicians Network (PPN) flowcharts for diagnosis and treatment will help clinicians evaluate their patients and determine the best course of treatment. Guidelines and workflows were approved by practitioners of the PANDAS Physicians Network Scientific Advisory Board. More detailed resources are available at www.pandasppn.org. Diagnosing and treating should be done by a licensed healthcare provider.
Primary care providers play important, ongoing roles in the diagnosis, treatment, and recovery of children with PANS/PANDAS (Pediatric Acute-onset Neuropsychiatric Syndrome / Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections). Children with a moderate or severe/life threatening onset or a complex presentation may require treatment by an experienced multi-disciplinary team of specialists or a PANS/PANDAS specialist. Additional resources can be found at www.pandasppn.org/practitioners.
Quick references:
- PANDAS Physicians Network website: www.pandasppn.org
- Seeing Your First Child with PANDAS/PANS: www.pandasppn.org/seeingyourfirstchild
- Treatment providers: www.pandasppn.org/practitioners
- Symptom severity definitions: www.pandasppn.org/symptom-severity
Treatment Guidelines
PANS/PANDAS TREATMENT GUIDELINES: MILD CASE
Mild: Symptoms are significant and cause disruptions at home and/or school. They occupy a few hours a day.
INITIAL EVALUATION AND TREATMENT
- Perform a comprehensive laboratory and clinical evaluation.
- Look for infections (Throat swab/culture child and family members for strep, check for exposure to Group A Streptococcus through close contacts, inquire about perianal redness or itching which may indicate perianal strep, and check for mycoplasma or other infections, e.g., yeast).
- While waiting for lab results:
- Prescribe 14 days of antibiotics (Penicillin/amoxicillin,¹ azithromycin, cefdinir, Augmentin, or others).
- Consider a 5-7 day course of NSAIDs at immunomodulatory dose for 24 hour coverage.² (see resource page)
- Ensure the family has access to CBT/ERP (Cognitive Behavior Therapy/Exposure and Response Prevention) and parent support.
- Schedule a follow up appointment.
FIRST FOLLOW-UP ASSESSMENT
- If significant improvement:
- No further intervention is needed at this time.
- Schedule a follow-up appointment within 30 days (or earlier if symptoms return).
- If no improvement:
- Look again for infection (i.e., swab/culture child and family members, check for mycoplasma or other infections).
- Check for sinusitis and consider a perianal strep swab.
- Consider changing antibiotic (change to azithromycin, cefdinir, or Augmentin).
- Consider a 5 day steroid burst³ or extend course of immunomodulatory dose of a NSAID.² (see resource page)
- Ensure the family has access to CBT/ERP. If the child is not able to engage in CBT/ERP due to the severity of symptoms, learning parent management techniques may be beneficial for the family.
- Consider a referral with a psychiatrist to help with symptom management.
- Schedule a follow-up appointment.
SECOND FOLLOW-UP ASSESSMENT
- If there was significant improvement between visits, but active symptoms:
- Recheck for active infection and exposure from siblings, parents, and close contacts.
- Restart antibiotics for 14 days and schedule a follow up appointment.
- If child has 2+ recurrences, consider prophylactic antibiotics¹. (see resource page)
- If no improvement:
- Consider a 5 day steroid burst³ or extend course of immunomodulatory dose of a NSAID.² (see resource page)
- Determine if symptoms have worsened to the point of being moderate or severe/life threatening.
- Ensure the family has access to CBT/ERP. If the child is not able to engage in CBT/ERP due to the severity of symptoms, learning parent management techniques may be beneficial for the family.
- Consider a referral with a psychiatrist to help with symptom management.
- Re-evaluate for possible alternative diagnosis.
PANS/PANDAS TREATMENT GUIDELINES: MODERATE CASE
Moderate: Symptoms are distressing and interfere with daily activities. They occupy 50%–70% of waking hours.
INITIAL EVALUATION AND TREATMENT
- Perform comprehensive laboratory and clinical evaluation.
- Look for infections (Throat swab/culture child and family members for strep, check for exposure to Group A Streptococcus through close contacts, inquire about perianal redness or itching which may indicate perianal strep, and check for mycoplasma or other infections, e.g., yeast).
- Perform additional laboratory testing to rule out other conditions and guide treatment.
- While waiting for lab results:
- Prescribe antibiotics (Penicillin/amoxicillin,¹ azithromycin, cefdinir, Augmentin, or others). Consider an initial 3-4 week course.
- Prescribe a steroid burst³ or a 5-7 day course of NSAIDs at immunomodulatory dose.² (see resource page)
- Ensure the family has access to CBT/ERP. If the child is not able to engage in CBT/ERP due to the severity of symptoms, learning parent management techniques may be beneficial for the family.
- Consider a referral with a psychiatrist to help with symptom management.
- Schedule a follow-up appointment.
FIRST FOLLOW-UP ASSESSMENT
- If significant improvement:
- Schedule another follow-up appointment and monitor for recurrence.
- If no improvement:
- Prescribe alternate antibiotic (change to azithromycin, cefdinir, or Augmentin).
- Check for sinusitis and consider a perianal strep swab.
- If not tried, prescribe a 5 day steroid burst³ or 6 weeks of a NSAID at immunomodulatory dose.² (see resource page)
- Consider MRI and EEG study.
- Consider checking antinuclear antibody titers, cross-reactive antineuronal antibodies, and CaM Kinase II activation.⁴ (see resource page)
- Schedule a follow-up appointment.
SECOND FOLLOW-UP ASSESSMENT
- If no current symptoms:
- Continue to monitor for subsequent exacerbations.
- Advise parents to continue with CBT/ERP.
- If child has 2+ recurrences, consider prophylactic antibiotics.¹ (see resource page)
- If active symptoms, but significant improvement between visits:
- Recheck for active infection and exposure from siblings, parents, and close contacts.
- Restart antibiotics for 14 days and schedule follow-up appointment.
- Consider 30 days of a steroid with taper.³ Continue antibiotics while the patient is taking a steroid. (see resource page)
- Schedule IVIG (1.5-2g/kg over 2 days) and return visit 30 days post IVIG. Continue a treatment dose of antibiotics until IVIG treatment is completed. Prescribe prophylactic antibiotics post IVIG treatment.¹ (see resource page)
- Confirm the child is receiving CBT/ERP and/or psychiatric care; and discuss expectations of clinical outcomes.
- If no improvement:
- Determine if symptoms have worsened to the point of being severe or life threatening.
- Consider an emergency referral with a psychiatrist to help with symptom management.
- Continue antibiotics. Total duration of antibiotic treatment is at least 30 days.
- Try 30 days of a steroid with taper.³ Continue antibiotics while the patient is taking a steroid. (see resource page)
- Refer patient to ENT for evaluation of tonsils and adenoids.
- Schedule IVIG (1.5-2g/kg over 2 days) and return visit in 30 days post IVIG. Continue a treatment dose of antibiotics until IVIG treatment is completed. Prescribe prophylactic antibiotics post IVIG treatment.⁴ (see resource page)
- Confirm the child is receiving CBT/ERP and/or psychiatric care; and discuss expectations of clinical outcomes.
POST IVIG APPOINTMENT
- If substantial improvement or fully improved:
- Advise parents to continue with CBT/ERP for any residual symptoms.
- Prescribe long-term prophylactic antibiotics post IVIG treatment.¹ (see resource page)
- If modest improvement:
- Advise parents to continue with CBT/ERP.
- Prescribe long-term prophylactic antibiotics post IVIG treatment.¹ (see resource page)
- Continue to monitor for symptom flares.
- If no improvement:
- Re-run diagnostic tests and determine if symptoms have worsened to the point of being severe or life threatening.
- Consider a second IVIG or a referral to a center to evaluate for plasmapheresis. Prescribe prophylactic antibiotics while coordinating care.¹ (see resource page)
- Advise parents to continue with CBT/ERP.
- Re-evaluate for possible alternative diagnosis.
PANS/PANDAS TREATMENT GUIDELINES: SEVERE/EXTREME CASE
Severe/Extreme: Symptoms are incapacitating, life threatening, or occupy 71%–100% of waking hours.
INITIAL EVALUATION AND TREATMENT
- Perform comprehensive laboratory and clinical evaluation.
- Look for infections (Throat swab/culture child and family members for strep, check for exposure to Group A Streptococcus through close contacts, inquire about perianal redness or itching which may indicate perianal strep, and check for mycoplasma or other infections, e.g., yeast).
- Order additional laboratory testing to rule out other conditions and guide treatment.
- For patients experiencing ARFID (Avoidant/Restrictive Food Intake Disorder), evaluate to determine if hospitalization is needed due to dramatic weight loss or if intravenous hydration is required.
- Prescribe a steroid burst³ or a 5-7 course of NSAIDs at immunomodulatory dose.² (see resource page)
- Begin scheduling for IVIG (1.5-2g/kg over 2 days).
- Prescribe antibiotics (Penicillin/amoxicillin¹, azithromycin, cefdinir, Augmentin, or others). Consider an initial 3-4 week course.
- Consider a referral with a psychiatrist to help with symptom management.
- Schedule telephone check-in and schedule a follow-up visit.
PHONE CHECK-IN
Monitor progress approximately 5 days after initial evaluation via a phone check-in.
- If significant improvement:
- Ensure the family has access to CBT/ERP. If the child is not able to engage in CBT/ERP due to the severity of symptoms, learning parent management techniques may be beneficial for the family.
- Confirm a follow-up visit is scheduled.
- If no improvement at phone check-in:
- Consider prolonged steroids (30 days) with taper.³ Continue antibiotics while the patient is taking steroids. (see resource page)
- Consider switching antibiotics (to azithromycin, cefdinir, or Augmentin).
- Refer patient to ENT for evaluation of tonsils and adenoids.
- Consider proceeding with IVIG treatment (1.5-2g/kg over 2 days).
- Based on the situation/safety, consider inpatient hospitalization or a center specializing in neuroimmune disorders.
- Confirm a follow-up visit is scheduled.
FOLLOW UP APPOINTMENT
- If significant improvement:
- Consider long-term prophylactic antibiotics.¹ (see resource page)
- If NSAIDs were prescribed, continue at immunomodulatory dose for a total of 6-8 weeks.² (A Proton Pump Inhibitor (PPI), such as omeprazole, lansoprazole, pantoprazole, or oresomeprazole, should be considered at prescribed dosages throughout the course of NSAIDs to prevent GI complications.) (see resource page)
- If improved, but not back to baseline, schedule IVIG (1.5-2g/kg over 2 days) and follow-up visit at 30 days. Continue a treatment dose of antibiotics until IVIG treatment is completed. Prescribe prophylactic antibiotics post IVIG treatment.¹ (see resource page)
- If no improvement:
- Change antibiotic (to azithromycin, cefdinir, or Augmentin). Total duration of antibiotic treatment is at least 30 days.
- Check for sinusitis and consider a perianal strep swab.
- Prescribe prolonged steroid (30 days) with taper.³ Continue antibiotics while the patient is taking steroids. (see resource page)
- Consider checking antinuclear antibody titers, cross-reactive antineuronal antibodies, and CaM Kinase II activation.⁴ (see resource page)
- Based on situation/safety refer for inpatient help or a center specializing in neuroimmune disorders.
- Schedule IVIG (1.5-2g/kg over 2 days) and follow-up visit at 30 days. Continue a treatment dose of antibiotics until IVIG treatment is completed. Prescribe prophylactic antibiotics post IVIG treatment.¹ (see resource page)
POST IVIG APPOINTMENT
- If fully improved:
- Refer to a PANS knowledgeable therapist for CBT/ERP treatment for residual symptoms and for managing flare-ups.
- Prescribe long-term prophylactic antibiotics post IVIG treatment.¹ (see resource page)
- If modest improvement (reduction of <50% of symptoms):
- Refer to a PANS knowledgeable therapist for CBT/ERP for treatment for residual symptoms.
- Prescribe long-term prophylactic antibiotics post IVIG treatment.⁴ (see resource page)
- Consider scheduling second IVIG for 90 days from initial IVIG.
- If no improvement:
- Consider a referral to a center for plasmapheresis. Prescribe prophylactic antibiotics while coordinating care.¹ (see resource page)
- Consider other treatment options (see text on www.pandasppn.org).
- Refer to a center specializing in neuroimmune disorders.
- Re-evaluate for possible alternative diagnosis.
PANS: Pediatric Acute-onset Neuropsychiatric Syndrome
PANDAS: Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections
CBT: Cognitive Behavioral Therapy
ERP: Exposure Response Prevention
IVIG: Intravenous immunoglobulin
NSAID: Nonsteroidal anti-inflammatory drugs
PEX: Plasmapheresis / Plasma Exchange
Resources
Reference: Journal of Child & Adolescent Psychopharmacology. Sept 2017. 27(7) pandasppn.org/jcap2017
¹ Bacteriologic and clinical treatment failures can occur with any antibiotic (i.e., The failure rate for penicillin therapy for strep is approximately 30%.*). If your patient is prescribed a prophylactic antibiotic and experiencing a subsequent onset of neuropsychiatric symptoms, consider the possibility of breakthrough strep. *Pichichero ME et al. Penicillin failure in streptococcal tonsillopharyngitis: causes and remedies, Pediatr Infect Dis J.2000 Sep;19(9):917-23.
² NSAID dosing can be found in Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome: Part II—Use of Immunomodulatory Therapies, Appendix Table A1.Use of Nonsteroidal Anti-Inflammatory Drugs in Pediatric Acute-Onset Neuropsychiatric Syndrome https://doi.org/10.1089/cap.2016.0148. A Proton Pump Inhibitor (PPI), such as omeprazole, lansoprazole, pantoprazole, or oresomeprazole, should be considered at prescribed dosages throughout the course of NSAIDs to prevent GI complications. Ensure proper hydration during the course of NSAIDs.
³ Long term corticosteroids are contraindicated for some patients. Screen for TB, Lyme, parasites, & fungi before prescribing. If patient responds to a 5 day steroid burst, this indicates an inflammatory/autoimmune process. Lack of significant improvement does not dismiss the possible correlation.
⁴ Chain JL, et al. (2020) Autoantibody Biomarkers for Basal Ganglia Encephalitis in Sydenham Chorea and Pediatric Autoimmune Neuropsychiatric Disorder Associated With Streptococcal Infections. Front. Psychiatry 11:564. doi: 10.3389/fpsyt.2020.00564. For information on The Autoimmune Brain Panel™ by Moleculera Biosciences, Inc., visit https://www.moleculera.com.
The diagnostic flowchart and treatment guidelines should be considered “living documents” that are open for revisions and updates as new research is published. CLICK HERE to leave comments or feedback. Thank you.
PANDAS PHYSICIANS NETWORK | www.pandasppn.org/flowchart | Version 1